In the last six years, Luanna Larusson has seen her 22-year-old daughter overdose multiple times, sleep on the streets and walk out of the hospital with an intravenous port still stuck in her arm.
The Langford mother says anyone who argues that no one who is severely addicted or mentally ill should be taken into care against their will should talk to parents like her.
“Unless you’ve walked in those shoes, unless you’ve walked that path with your son or daughter or mother or father or anyone in your family, you won’t know the extent of that person’s life, if it’s called a life,” said Larusson, who wrote to Premier David Eby, government ministers and Community Living B.C. this week detailing her family’s struggles.
“I used to walk downtown in the middle of the night looking for her, absolutely terrified that I would find her naked body under a bush, her floating in the Inner Harbour or some man doing horrible things to her.
“It’s either recovery or death.”
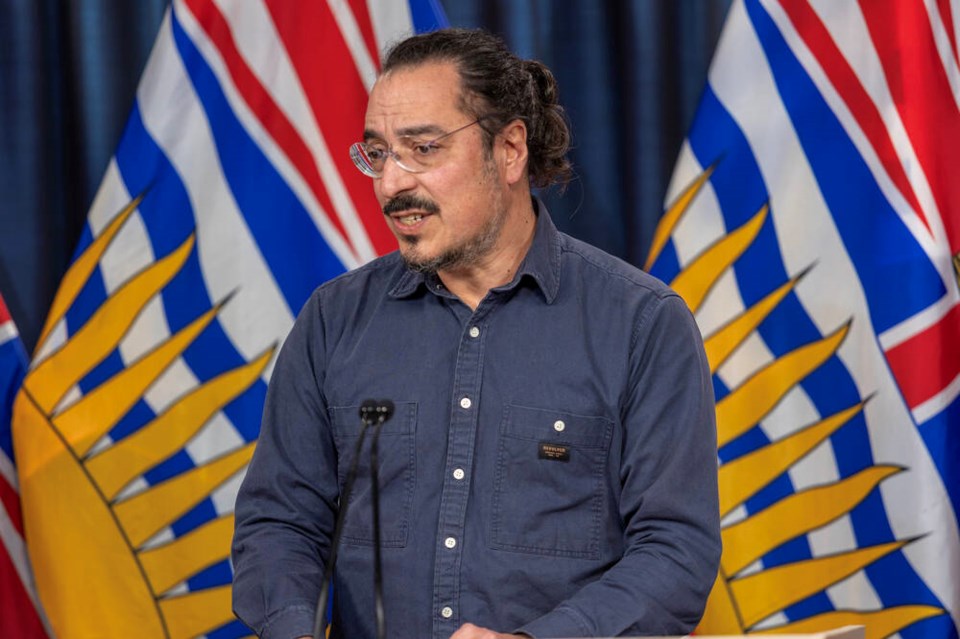
Psychiatrist Dr. Daniel Vigo, the province’s scientific adviser for psychiatry, toxic drugs and concurrent disorders, announced this week that new involuntary care beds will open at Surrey Pretrial Services this month “for those in conflict with the law,” and at Alouette Homes in Maple Ridge later this spring for those with the most severe behavioral challenges resulting from concurrent disorders.
He also released updated guidelines to clarify how the Mental Health Act allows for involuntary care of people with concurrent mental health, acquired brain injury and substance-use disorders.
Larusson, 68, whose husband died in 1988, had already raised her two daughters, now 42 and 43, when during a volunteering stint for an AIDS organization in South Africa she offered to help a struggling 16-year old mother and father by taking their six-week old daughter for the weekend.
Come Monday when she went to return the baby, they wouldn’t take her. Larusson couldn’t leave her behind.
The widowed mother adopted baby Elihle, whose birth name in Xhosa means “beautiful.”
“I just couldn’t imagine turning my back on her,” said Larusson, who says she obtained her daughter’s permission to tell her story. “I love her so much. I brought her to Canada with this idea I would give her a different life.”
When she was 16, Elihle tried to keep up with her peers and school work, but following a falling out with her friends, while her mom was working full time, she headed downtown and found the wrong type of friends, who introduced her to drugs. She’s now addicted to fentanyl and methamphetamines.
“She had an almost fatal overdose three weeks after being introduced to heroin,” said Larusson. “She overdosed again two months later. She was discharged from hospital to youth detox, but did not stay.”
It wasn’t until Larusson had her daughter tested at Queen Alexandra Centre for Children’s Health in Saanich that she was diagnosed with Fetal Alcohol Spectrum Disorder and other cognitive impairments.
Passed ‘around and around and around’
Over more than six years, Elihle has been in the care of various ministries, outreach programs and complex-care teams, said Larusson.
She stayed at a Central Saanich group home for four months until she ran away and camped out in a tent at Centennial Square. She also ran away from a group home closer to town.
Once, she became “violent, physically and verbally abusive, and threatened to kill me and then herself,” said Larusson.
Her daughter was finally admitted to hospital under the Mental Health Act but discharged days later and advised to go for counselling, “but the counsellor said she couldn’t do much for her if all she did was cry during sessions.”
Elihle was prescribed an antidepressant, but then overdosed on the medication.
After refusing treatment, she was put in another group home, but again returned to street encampments.
When the pandemic hit and hotels were opened to house the homeless, Elihle was placed in the Howard Johnson Hotel on Gorge Road. Her mother stayed with her then 17-year-old daughter to protect her as much as she could. Elihle ended up staying in the hotel for three years.
“I warded off advances from men who came to her room at all hours of the night with drugs,” said Larusson. “There were drug dealers in the building so she didn’t have to leave.”
She was relocated to the tiny home community at Royal Athletic Park, but left. She ended up at newly built supportive housing on Meares Street — a partnership between the province and the city — but staff reported that out of 400 days, she was seen at the building maybe 40 times.
She’s now been given a month to either spend at least two nights out of seven at Meares — where a strict no-visitor policy prevents even her mother from checking on her — or be transferred to a shelter.
“I don’t understand how people who work in the addiction field can say that people under the influence of fentanyl can make decisions when chasing the fentanyl is their only priority,” said Larusson, who describes herself as her daughter’s “external brain” for 16 years — even before addiction.
She says her daughter can in no way look after herself, whether it’s cooking, bathing, finances, planning or health care, noting she has lost or traded more than 20 cellphones, lost her bank card as many times, and spends her disability money within a week on drugs.
Larusson, who drives around with clothing and supplies in her vehicle in case she sees her daughter, says she can pull up to a downtown street and people will call out to Elihle: “your mom is here” — just as a school friend or neighourhood playmate might announce an arriving parent at pick-up time.
Her mother says Elihle has had cellulitis in the palm of her hand and dental abscesses that rendered her unable to eat and talk, and has been physically assaulted by a “boyfriend,” requiring 15 stitches just below her eye.
She said she has spent hours downtown looking for her daughter just to administer antibiotics three times a day because she wasn’t able to do it herself. “She left the hospital while being treated for the cellulitis, removing the IV line herself, but the IV port remained in her forearm for 10 days before I could find her and have it removed.”
Larusson said she feels hopeless, passed “around and around and around” from government ministries to organizations and housing sites. And now she’s frightened that her daughter will be discharged to a shelter bed if she doesn’t comply with the rules of her supportive housing unit.
Larusson said if her daughter had secure care in the beginning, she might have avoided the pain of the last six and a half years.
The one time her daughter was sober, she said, was when she was sent to Burnaby youth custody, a secure facility with three meals a day, chores to earn money, safe sleeping quarters, no drugs, and someone else making decisions for her.
“She thrived,” said Larusson. “She said she loved it there.”
While Larusson has support from her daughters and close friends, at nearly 70 years old and with compromised health, she worries about who will care for her daughter when she’s not able to.
“I’ve been following my daughter for six and a half years, and I’ve been with her every step of the way. I’ve been to meetings, I’ve been waving the flags. I’ve been saying she’s not able to make those decisions, and I’ve been ignored for the most part, and I feel very frustrated and hopeless.
“I feel like I’m a voice in the wilderness.”
‘I fear for her life every day’
Health Minister Josie Osborne this week called the opening of two involuntary care facilities on the Lower Mainland an “important step,” saying the province is also working on providing more voluntary recovery and treatment beds.
Larusson isn’t sure if her daughter would even qualify for involuntary care. Last September, an emergency-room physician told Larusson her daughter “wasn’t bad enough to commit her under the Mental Health Act.”
Vigo said the threshold for involuntary care is that a person has a mental disorder that seriously impairs their ability to engage with others and their environment, they require treatment to prevent their substantial physical or mental deterioration or for the protection of themselves or others, and the person is not suitable for voluntary admission. He has said that only a couple of hundred people in the province would fall into that category.
While substance-use disorder is a mental-disorder subtype, a mental disorder alone is not grounds for involuntary treatment for 99 per cent of those patients, Vigo said.
Some advocates for those with mental health and addictions have criticized involuntary care, saying only those who voluntarily seek treatment stand a chance of benefiting from it — and that it could even be harmful if those forced into detox later return to the streets, only to overdose because their drug threshold isn’t as high as it was.
In September, the Canadian Mental Health Association criticized the province’s plan to expand involuntary care, saying there has been a “dramatic increase” in reliance on involuntary services — with those with substance-use disorders the fastest-growing group being detained — while voluntary services have not kept up with demand.
Larusson, for her part, asks how her daughter could ever choose recovery if “she is unable to choose something as simple as brushing her teeth, or spend the night at Meares in order to prevent herself from being evicted.”
She said she’s frustrated with organizations expecting her daughter to voluntarily make changes, assuming that “one day she will wake up and decide that today is the day.”
She dreams of her daughter detoxing and getting the months and maybe years of therapy she needs.
“She has the right to achieve her full potential,” Larusson said, but “while we continue to enable her drug addiction, we take away her right to a healthy life.”
Asked by the Times Colonist for her own views on involuntary care, Elihle said: “I wouldn’t like it but I would understand.”
“I wouldn’t feel like it’s completely against my will, because that would be just kind of silly because the whole point is to live, right?”
While Larusson is not sure if involuntary care would even work for her daughter, she is sure of one thing: What she has been offered for almost seven years “has definitely not worked.”
“I fear for her life every day,” she said. “I fear that I’m going to get that phone call — or the police knocking at my door — to say that she’s gone.”